Keratoconus
Definition
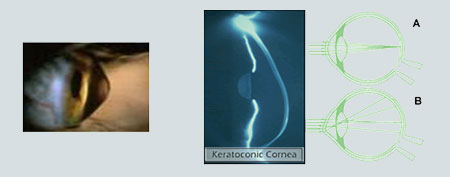
Keratoconus is a non-inflammatory, progressive eye disorder which is considered a corneal ectasia and in which the cornea is deformed and takes a conical form.
It is characterized by:
- Central or paracentral thinning of the layer, resulting in the reduction of the corneal thickness to 1/3 of its normal thickness.
- Development of irregular astigmatism
- Conical protrusion of the cornea, usually peripherally and in the lower part.
The evolution of the disease leads progressively to the reduction of visual acuity and to the reduction of visual quality, phenomena that cannot be improved using corrective glasses.
This condition is considered hereditary and its occurrence has been attributed to several factors over time; abnormalities in the structure and metabolism of various parts of the cornea are mainly held responsible for the condition.
In Greece, it is estimated that the incidence rate of this disease is 1 in 2,000 people, or a total of about 20,000 people. It has been observed that it begins at puberty, progresses rapidly and then decelerates until it stops at about 35 years of age.
Keratoconus
Keratoconus – Symptoms
In most cases, keratoconus does not show any symptoms and the disease is usually diagnosed during a pre-operative evaluation prior to refractive surgery.
The first symptoms suggesting the occurrence of keratoconus are frequent changes of prescription glasses and blurry vision, which cannot be regulated by corrective glasses due to constantly increasing myopia and astigmatism.
Other symptoms include:
- Headaches
- Eye irritation
- Increased photosensitivity
- Decreased visual acuity.
- Difficulty in night driving
- Intolerance to soft contact lenses
- Halos, double vision in one eye or even light diffractions at night.
- Irregular astigmatism that cannot be corrected through corrective glasses
- Sudden decrease in vision due to hydrops
It is very difficult to diagnose keratoconus during the early stages of the disease, as the symptoms mentioned above may relate to other ophthalmological conditions as well. In any case, you should consult your ophthalmologist to diagnose this condition.
Keratoconus – Diagnosis
The following examinations are necessary for the diagnosis of keratoconus:
- Corneal Topography: During this examination, we make a two-dimensional imaging of the morphology of the cornea and use it to diagnose even the subclinical forms of the disease, i.e. the cases, where are no symptoms yet. In keratoconus, the topographical color maps offer information about the site, curvature and size of the top of the cone. Our topography systems can also examine the curvature of the posterior surface of the cornea, the abnormalities of which seem to precede the abnormalities of the anterior. Finally, during the same examination, we measure accurately the thickness of every point of the cornea.
- Keratometry: This examination is used to initially diagnose irregular astigmatism, as the main meridians are not separate by 90˚ and the images of the keratoscopes cannot fall on top of one another. Also, per the values of keratometry, keratoconus is considered mild if it is less than 48D, moderate between 48-54D and advanced if it is above apo54D.
- Direct ophthalmoscopy: An oil droplet reflex is observed
- Skiascopy: Shows irregular scissoring reflections.
- Photokeratoscopy: Shows irregularities on the rims of the rings.
